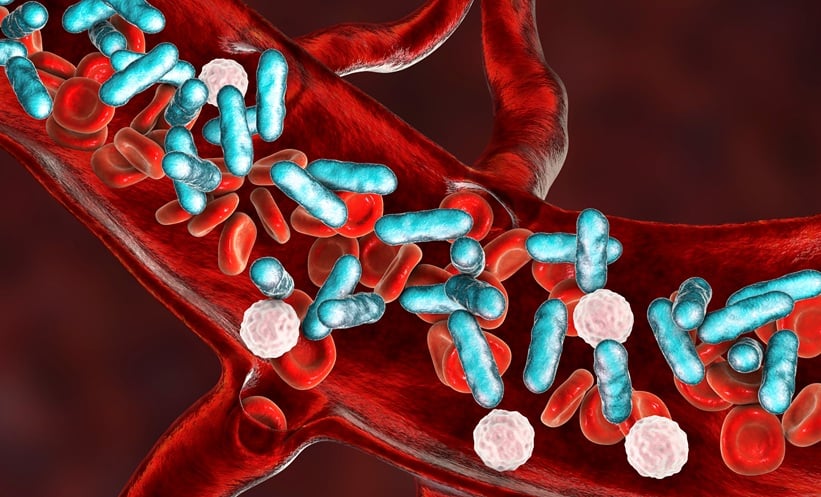
SEPTIC shock is the most severe form of sepsis, occurring when a widespread infection leads to dangerously low blood pressure, organ failure and a high risk of death. Despite advances in intensive care, mortality remains substantial. A major new systematic review and meta-analysis sheds light on which patients are most likely to die early, offering clinicians clearer guidance for risk assessment and decision-making.
Why Early Mortality in Septic Shock Matters
Early mortality, defined as death during hospitalisation or within 31 days, affects roughly one in three patients with septic shock. Identifying prognostic factors early could support more informed goals-of-care discussions, prioritise resources, and help tailor treatment intensity for those at highest risk. To address this, researchers analysed data from nearly 5 million patients across 95 studies, making this one of the largest evaluations of early mortality in septic shock to date.
Patient Characteristics Linked To Septic Shock Outcomes
Several patient-level factors were consistently associated with a higher risk of early death in septic shock. Increasing age was linked to rising mortality, even when adjusted for other factors. Comorbidities played a major role: patients with liver cirrhosis, cancer, or a higher Charlson comorbidity index faced substantially worse outcomes.
The analysis also found higher mortality among Black patients compared with other racial groups, highlighting ongoing disparities in outcomes that warrant further investigation but should not be interpreted as causal.
Severity at Presentation Signals Risk
Clinical severity on admission emerged as a strong predictor of outcome in septic shock. Acute kidney injury nearly doubled the risk of early death. Established severity scoring systems used in intensive care, including APACHE II, SAPS II, and SOFA scores, were all strongly associated with mortality, reinforcing their value in bedside prognostication. For clinicians, these scores provide a practical way to contextualise risk during the initial assessment.
Treatments and Biomarkers Associated with Mortality
Certain treatments and laboratory markers were also linked with poorer outcomes. The need for invasive mechanical ventilation and use of norepinephrine, a marker of circulatory failure severity, were associated with higher mortality. Elevated serum lactate levels, reflecting impaired tissue oxygenation, were another strong predictor.
Importantly, these associations likely reflect illness severity rather than harm from the treatments themselves.
Implications for Clinical Practice
This analysis does not change how septic shock should be treated, but it clarifies which factors are most informative for early risk stratification. By integrating patient history, severity scores and key biomarkers, clinicians may better identify patients at highest and lowest risk, supporting personalised care planning and clearer communication with patients and families.
Reference
Jung RG et al. Prognostic factors associated with mortality in septic shock: a systematic review and meta-analysis. Lancet Respir Med. 2026; DOI:10.1016/S2213-2600(25)00397-2.